Skip to site content
Total hip arthroplasty, also known as hip replacement surgery, accounts for an astonishing 330,000 procedures in the U.S. annually. Orthopedic surgeons remove diseased hip joints and replace the parts with prosthetic ones.
Patients and providers agree that hip replacement surgeries generally prolong mobility and improve quality of life. Controversy recently emerged over which arthroplasty approach is optimum. Do the benefits of anterior hip replacement outweigh the risks?
Prior to hip replacement, clinicians frequently recommend their patients pursue noninvasive treatments. Pain management, physical therapy and assistive devices often reduce joint pain, improve mobility and postpone surgery. Thorough pre-operative interventions also include lifestyle modifications.
When these treatment modalities are ineffective, it’s likely time to consider joint replacement. Common diagnoses that warrant hip arthroplasty are the following:
The first groundbreaking “total extirpation of articulation,” or hip replacement, was performed by Dr. Henry Park in the 18th century. During that time, war and violent conflict were prevalent in Europe. Limb amputation was a common practice in treating war victims. Many surgeons were horrified at the thought of joint arthroplasty. Yet, Dr. Park courageously fought to save limb and life.
Today, we aim higher. Not only do surgeons strive to spare the diseased limb, but they are also concerned about protecting muscles and tendons. Scientists and surgeons push for innovations that improve outcomes and longevity of the joint.
Patients have come to expect shorter hospital stays and quick recoveries. Surgeons no longer wonder if they can perform a hip replacement but instead if they can perform it better than their predecessors.
With minimally invasive techniques, smaller equipment and innovative approaches, patients boast about phenomenal results. They often wish they had done the replacement sooner.
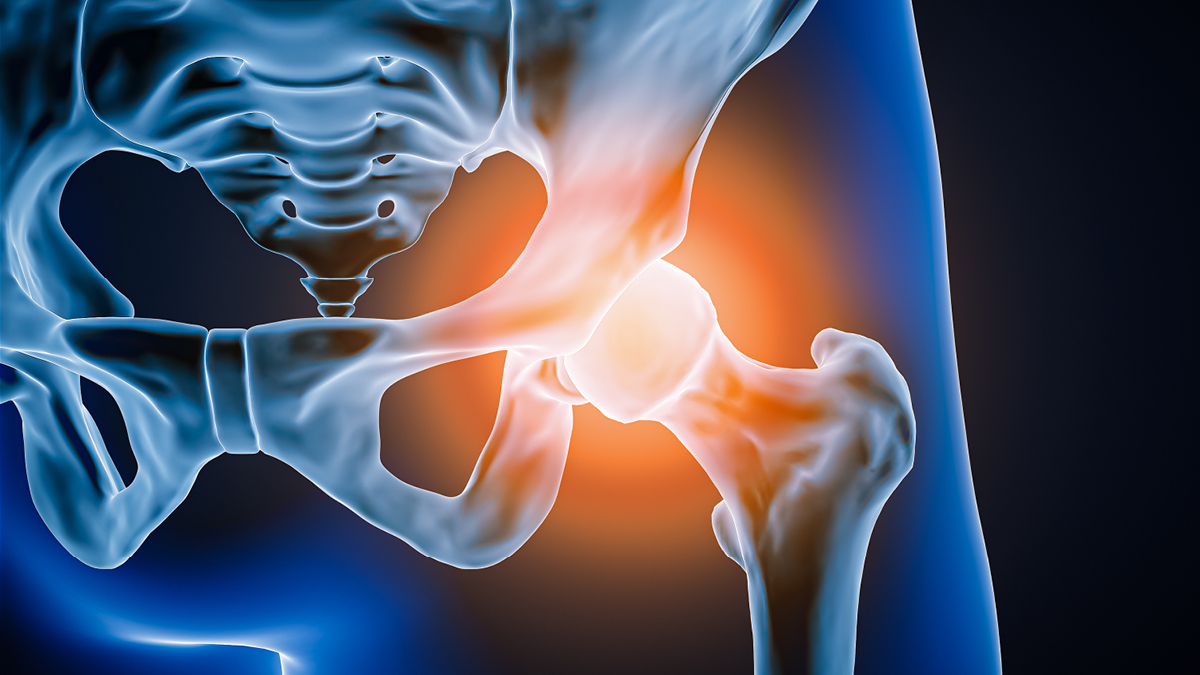
Yes, research indicates that technique and surgical approach matters for hip replacements. Since the hip is a ball-and-socket joint, the femoral head naturally fits inside the pelvic bone’s acetabulum, the socket portion of the hip.
An incision allows surgeons to remove the diseased bone and replace the femoral head and acetabulum with a new, artificial joint. Traditionally, surgeons cut an incision behind the joint (posterior approach) or on the side of the hip (lateral approach).
However, research indicates improved results with an incision at the front of the hip joint (anterior approach). This approach allows for a smaller incision, reducing trauma to the muscles and tendons surrounding the joint.
Since the direct anterior approach (DAA) is less invasive than the mini-posterior approach (MPS), patients and providers notice the benefits of anterior hip replacement.
With DAA, patients show improved functional milestones within four to five days. Research proves that anterior hip replacement reduces recovery times and promotes faster milestone achievements. One-year joint arthroplasty success rates are similar regardless of the location of the incision.
The anterior approach requires more than just a change of incision location. Surgeons need specialized training for appropriate execution and avoidance of complications. A high BMI (>30 kg/m2), more than three comorbidities or pelvic anatomy variations contraindicate the use of DAA. Complication risks for DAA are the same as other arthroplasty approaches:
The length of hospital stay after a hip replacement varies. Some physicians perform anterior hip replacements as an outpatient procedure and discharge people that same day. Other patients can expect one to two days in the hospital.
When planning for discharge, patients must arrange for someone to take them home. Otherwise, providers require hospitalization.
Committing to physical therapy is vital. Improved strength and mobility depend on it. Doctors may also recommend occupational therapy to aid with daily activities, like getting dressed or bathing.
Your patients can expect four to six weeks of therapy before they can independently perform daily activities. When support is lacking at home, rehabilitation facilities ensure post-op patient safety, PT and OT.
Most people return to their routine after a month. If your patient’s work requires extensive standing, walking or lifting, encourage them to allow approximately three months before returning to work.
Over the years, innovations have raised the bar for all surgical procedures. Minimally invasive surgical techniques, like anterior hip replacement, are the gold standard of evidence-based practices. However, anterior hip arthroplasty should only be performed by an experienced hand.
“Hip Replacement Surgery.” NIH: National Institute of Arthritis and Musculoskeletal and Skin Disease, 2023, Hip Replacements – What to Expect & How to Prepare | NIAMS.
“Orthopedic Surgery.” Mayo Clinic, 2017, Direct anterior hip arthroplasty – Mayo Clinic.
“Historical overview of hip arthroplasty: From humble beginnings to a high-tech future.” NIH: National Library of Medicine, 2021, Historical overview of hip arthroplasty: From humble beginnings to a high-tech future – PMC.
“Direct anterior approach in total hip arthroplasty: more indications and advantages than we found.” Arthroplasty, 2022, Direct anterior approach in total hip arthroplasty: more indications and advantages than we found | Arthroplasty | Full Text.
Subscribe to our MEDforum e-newsletter for the latest guidelines and information from Up Health.